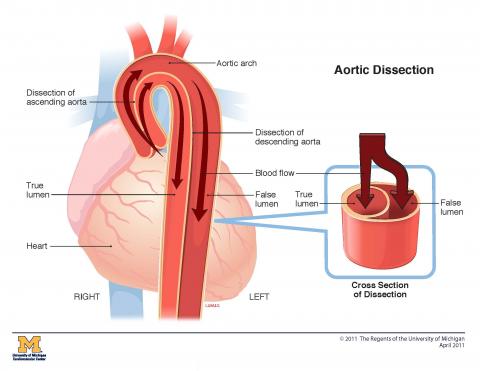
An aortic dissection occurs when the inner layer of the aortic wall tears. The inner and middle layers of the aorta separate and fill with blood, weakening the wall of the aorta. If pressure builds up, it can lead to a dangerous rupture where blood spills inside the body.
When you come to the University of Michigan Health Frankel Cardiovascular Center, you’ll find experts with decades of experience diagnosing and treating aortic dissections. We are the primary center in the region for complex dissections, offering lifesaving treatment to dozens of patients each year.
Aortic Dissection Care at the Frankel Cardiovascular Center
Within the Comprehensive Aortic Program, our unique team-based model of care provides
Types of Aortic Dissection
Your aorta is shaped like a cane. It starts at the aortic root where it meets the left ventricle of the heart (the main pumping chamber). The aortic valve sits within the aortic root and prevents blood from flowing backward. From there, the aorta travels up (ascends) toward the head, arches 180 degrees then travels down (descends) to the abdomen.
Aortic dissections are classified by their location:
Type A dissections occur in the ascending aorta.
Type B dissections occur in the descending aorta.
Causes
- Atherosclerosis (hardening of the arteries)
- Cocaine use
- High blood pressure
- Traumatic injury
- Aortic Aneurysms
- Genetics: Some people are born with a genetic predisposition for developing a dissection. If you have a parent or sibling with an aortic dissection, you are at higher risk. Aortic dissections are also associated with several genetic diseases and syndromes (for example, Marfan syndrome). If you have a dissection, your doctor will likely recommend meeting with our genetic counselors to discuss screening your family members.
Symptoms
The most common symptoms of an aortic dissection include:
- Difficulty speaking, loss of vision, weakness
- Fainting
- Shortness of breath
- Sudden, severe pain in the chest, back or abdomen
If you experience any symptoms, it is crucial to seek medical attention at the nearest emergency department. The University of Michigan collaborates with local and regional hospitals to provide transportation through our Survival Flight or ground transportation, as needed.
A dissection that occurs in an area of the aorta with branching arteries can block blood flow to the heart and brain, possibly leading to heart attack and stroke. Immediate treatment of dissections is critical for survival. Our Comprehensive Aortic Program is among the best in the nation for emergency care of patients with aortic dissections.
Diagnosis
To diagnose an aortic dissection, your doctor will ask about your medical and family history and perform a physical exam. Imaging tests help us confirm and locate the tear. These tests include:
- CT scan: This test uses powerful X-rays to produce cross-sectional views of the aorta.
- MRI: This scan uses a magnetic field and radio waves to produce detailed images of the aorta.
- TTE: Transthoracic echocardiogram
Treatment
The goals of aortic dissection treatment include:
- Treating complications, especially malperfusion syndrome which is the loss of blood supply to vital organs.
- Repairing the affected area
- Preventing further tearing, including medication to lower blood pressure and refraining from heavy lifting.
Acute Type A Dissection
Type A dissections usually require immediate repair. Our highly skilled surgeons are among the best in the country in repairing Type A dissections. We use grafts (fabric-covered, metal mesh tubes) to replace damaged areas of the aorta. While placing a graft, our doctors may perform additional procedures to improve your outcome. These complex surgeries are not available at most other hospitals. They include:
Open Surgical Repair of Type A Dissection
- Aortic root replacement and valve surgery – also called the Bentall procedure – replaces the aortic root plus the aortic valve. It is for patients who have an aortic root aneurysm or dissection plus aortic valve problems. This can be helpful for patients with aortic valve regurgitation (leaky valve) or calcification (hardening). The surgeon removes part of the aorta and the aortic valve, then replaces the missing section of the aorta with an artificial tube, called a graft. The aortic valve is replaced with a mechanical or biological valve. Patients with a mechanical valve must take blood-thinning medications for the rest of their lives to prevent blood clots from forming.
- Valve-sparing aortic root replacement: Valve-sparing aortic root replacement is a good choice if your aortic valve is working well. This procedure replaces your aortic root, but not your aortic valve. The Yacoub procedure involves remodeling the aortic valve. The David procedure involves reimplantation of your aortic valve. By keeping one's own valve, there is no need to take blood thinning medications for life.
- Aortic arch replacement: If a dissection involves the aortic arch, surgeons use a graft to replace the damaged area. Because major arteries branch off the aortic arch to the head, blood flow must be temporarily halted through a technique called hypothermic circulatory arrest to cool the body and interrupt blood flow. This preserves brain function. Once the graft is in place, surgeons reattach the arteries to the arch.
- Ascending aorta repair: In cases where the tear is located in the ascending aorta (the portion of the aorta that is closest to the heart), an open surgical procedure is performed. The procedure involves replacing the damaged section of the aorta with a synthetic graft or tube.
- Descending aorta repair: For dissections that occur in the descending aorta (the portion of the aorta that runs through the chest and abdomen), the damaged segment can be replaced or repaired using open surgery techniques.
- Frozen elephant trunk procedure: This procedure is used for complex aortic pathologies that involve both the ascending (near the heart), arch, and descending (farther down the chest and into the abdomen) segments of the aorta. The surgeon will repair or replace the damaged portion of the aorta. The "elephant trunk" component of the procedure involves a stent to cover the portion of the aneurysm that extends into the descending aorta. The stent graft helps to divert blood away from the dissected portion of the aorta. The term "frozen" in "frozen elephant trunk" refers to the fact that the distal end of the stent graft (the part that extends into the descending aorta) is positioned and secured within the aorta, effectively "freezing" it in place.
Malperfusion Management
Malperfusion syndrome, or lack of blood supply to vital organs, is the second most common lethal complication of acute aortic dissection following rupture. It occurs in 10% to 33% of all cases of both acute type A and type B dissection. Early diagnosis is essential. Patients who are at the highest risk of fatality from malperfusion are those with delayed diagnosis of dissection or delayed presentation to a medical center equipped to handle acute aortic dissection.
Malperfusion syndrome occurs when an aortic dissection blocks an artery that carries blood to a vital organ. Twenty years ago, Frankel Cardiovascular Center surgeons developed a world-renowned procedure using a laser inserted through a catheter to make holes in the blockages. This standard of care procedure restores blood flow, enabling surgical repair of the dissection and greatly improves survival.
Endovascular Treatment
Endovascular treatment for Type A aortic dissection are a relatively new and evolving approach to managing this life-threatening condition. Traditionally, Type A aortic dissections have been treated with open-heart surgery (aortic replacement), but endovascular techniques are being explored as alternatives in select cases. It's important to note that the choice between open surgery and endovascular therapy depends on various factors, including the patient's overall health, the extent of the dissection, and the experience of the medical team.
Open surgical repair remains the gold standard for many cases because it allows for complete removal of the dissected tissue and direct reconstruction of the aorta. Endovascular treatment for aortic dissections involves a catheter-based procedure to repair the affected section of the aorta. This helps to stabilize the aorta and prevent the tear from expanding further. This reduces the risk of rupture or occlusion. There are three main endovascular treatments: aortic stent-graft placement, dissection flap fenestration, and branch-vessel stenting. Typically, one or more of these endovascular techniques can be used to treat aortic dissection, and they may either complement surgical repair or make it unnecessary. Several clinical trials of endovascular treatments for aortic dissections are currently underway at the Frankel Cardiovascular Center.
Medical Management
Type A aortic dissection is a medical emergency and requires immediate intervention to prevent life-threatening complications. The primary treatment for Type A aortic dissection is typically surgical repair. However, before surgery can be performed, initial medical management may be crucial to stabilize the patient and manage pain. Here are the key aspects of medical management for Type A aortic dissection:
- Admission to the Intensive Care Unit (ICU): Patients with Type A aortic dissection are usually admitted to the ICU for close monitoring and immediate intervention if needed.
- Blood Pressure Control: One of the primary goals of medical management is to control blood pressure. High blood pressure can worsen the dissection by causing further tearing of the aortic wall. Medications such as intravenous beta-blockers (e.g., esmolol, labetalol) and vasodilators (e.g., sodium nitroprusside) are used to lower blood pressure and reduce the stress on the aortic wall.
- Pain Management: Severe chest or back pain is a common symptom of aortic dissection. Intravenous pain relievers, such as opioids (e.g., morphine), are administered to alleviate pain and keep the patient comfortable.
- Heart Rate Control: Tachycardia (rapid heart rate) can increase the force of blood against the weakened aortic wall. Medications like beta-blockers are used to control heart rate in addition to blood pressure.
- Monitoring: Continuous monitoring of vital signs, including blood pressure, heart rate, oxygen saturation, and electrocardiogram (ECG), is essential. Frequent imaging studies, such as CT angiography or transesophageal echocardiography (TEE), are performed to assess the extent of the dissection and guide treatment decisions.
- NPO Status: Patients are typically placed on "nothing by mouth" (NPO) status to prevent any food or fluids from being ingested until the surgical repair is completed.
- Preparation for Surgery: Medical management serves as a bridge to surgical intervention. Surgeons and the medical team work to stabilize the patient's condition, optimize blood pressure control, and ensure the patient is in the best possible state for surgery.
- Treatment of Complications: If complications arise during the initial management phase, such as organ malperfusion (inadequate blood supply to organs) or rupture, immediate intervention is necessary. Surgery may be expedited or performed as a life-saving measure.
- Multidisciplinary Care: The management of Type A aortic dissection requires a multidisciplinary approach involving cardiovascular surgeons, cardiologists, anesthesiologists, and critical care specialists who work together to coordinate care and make decisions based on the patient's individual condition.
It's important to note that while medical management is crucial in the early phase of Type A aortic dissection, it is not a definitive treatment. Surgical repair remains the standard of care, as it involves the removal of the dissected portion of the aorta and reconstruction of the aortic wall. The timing of surgery depends on factors such as the patient's stability, the extent of the dissection, and other individual characteristics, and it is determined by the medical team based on careful evaluation and monitoring.
Acute Type B Dissection
Open Surgical Repair of Type B Aortic Dissection
While medical management and TEVAR are the most common approaches to Type B aortic dissections, open repair may also be considered. This procedure can be performed to prevent complications and to stabilize the aorta in cases where medical management alone is insufficient. Open repair includes an incision that extends under the shoulder blade, around the side of the rib cage, to just under the breast. This lets the surgeon see the aorta directly to repair the aortic dissection.
Thoracic Endovascular Repair of Aorta (TEVAR)
Thoracic endovascular aortic repair (TEVAR) is a minimally invasive procedure used to repair a thoracic aortic aneurysm or dissection. TEVAR is an alternative to open surgery and can mean a shorter hospital stay and quicker recovery time. Since its approval by the Food and Drug Administration (FDA) in 2005, researchers have also documented better patient outcomes with TEVAR compared with open surgical repair.
Medical Management
Medical management of Type B aortic dissections aims to stabilize the patient's condition, control blood pressure, and reduce the risk of complications. Unlike Type A dissections, which often require immediate surgical intervention, Type B dissections are initially managed conservatively with medications and close monitoring. Here are the key components of medical management for Type B aortic dissections:
- Hospital Admission: Patients with Type B aortic dissections are usually admitted to the hospital, often to an intensive care unit (ICU) or a specialized vascular unit for close monitoring.
- Blood Pressure Control: Controlling blood pressure is a top priority in managing Type B dissections. The goal is to reduce the force of blood against the weakened aortic wall, which can help prevent further tearing of the aorta. Medications typically used for blood pressure control include:
- Beta-Blockers: These medications, such as labetalol or esmolol, are commonly used to slow the heart rate and reduce blood pressure. Beta-blockers decrease the shear stress on the aortic wall and help minimize the risk of dissection extension.
- Vasodilators: Medications like sodium nitroprusside may be used to relax blood vessels and lower blood pressure.
- Pain Management: Aortic dissections often cause severe chest or back pain. Intravenous pain relievers, such as opioids (e.g., morphine or fentanyl), are administered to alleviate pain and discomfort.
- Heart Rate Control: Tachycardia (rapid heart rate) can increase the force of blood against the aortic wall. Medications like beta-blockers are used to control heart rate in addition to blood pressure.
- Monitoring: Patients are closely monitored for any changes in blood pressure, heart rate, and overall clinical condition. Frequent imaging studies, such as computed tomography angiography (CTA) or magnetic resonance angiography (MRA), are performed to assess the extent of the dissection and to identify any complications.
- NPO Status: Patients are often placed on "nothing by mouth" (NPO) status to prevent any food or fluids from being ingested until their condition is stabilized and surgical intervention can be considered.
- Treatment of Complications: If complications arise during the initial management phase, such as organ malperfusion (inadequate blood supply to organs), rupture, or continued dissection extension, immediate intervention is necessary, and surgery may be considered.
- Multidisciplinary Care: Managing Type B aortic dissections often requires a multidisciplinary approach involving vascular surgeons, cardiologists, radiologists, and critical care specialists who collaborate to provide the best possible care and make informed decisions about the timing of surgical intervention.
The decision to proceed with surgery for Type B aortic dissections is based on various factors, including the patient's clinical condition, the extent of the dissection, the presence of complications, and individualized assessments by the medical team. In some cases, endovascular procedures like thoracic endovascular aortic repair (TEVAR) may be considered as an alternative to open surgery to treat specific segments of the dissection. Ultimately, the management approach should prioritize patient safety and optimize long-term outcomes.
Malperfusion Management
Malperfusion syndrome, or lack of blood supply to vital organs, is the second most common lethal complication of acute aortic dissection following rupture. It occurs in 10% to 33% of all cases of both acute type A and type B dissection. Early diagnosis is essential. Patients who are at the highest risk of fatality from malperfusion are those with delayed diagnosis of dissection or delayed presentation to a medical center equipped to handle acute aortic dissection.
Malperfusion syndrome occurs when an aortic dissection blocks an artery that carries blood to a vital organ. Twenty years ago, Frankel Cardiovascular Center surgeons developed a world-renowned procedure using a laser inserted through a catheter to make holes in the blockages. This standard of care procedure restores blood flow, enabling surgical repair of the dissection and greatly improves survival.
Chronic Aortic Dissection
Open Surgical Repair
- Aortic root replacement and valve surgery – also called the Bentall procedure – replaces the aortic root plus the aortic valve. It is for patients who have an aortic root aneurysm or dissection plus aortic valve problems. This can be helpful for patients with aortic valve regurgitation (leaky valve) or calcification (hardening). The surgeon removes part of the aorta and the aortic valve, then replaces the missing section of the aorta with an artificial tube, called a graft. The aortic valve is replaced with a mechanical or biological valve. Patients with a mechanical valve must take blood-thinning medications for the rest of their lives to prevent blood clots from forming.
- Valve-sparing aortic root replacement: Valve-sparing aortic root replacement is a good choice if your aortic valve is working well. This procedure replaces your aortic root, but not your aortic valve. The Yacoub procedure involves remodeling the aortic valve. The David procedure involves reimplantation of your aortic valve. By keeping one's own valve, there is no need to take blood thinning medications for life.
- Aortic arch replacement: If a dissection involves the aortic arch, surgeons use a graft to replace the damaged area. Because major arteries branch off the aortic arch to the head, blood flow must be temporarily halted through a technique called hypothermic circulatory arrest to cool the body and interrupt blood flow. This preserves brain function. Once the graft is in place, surgeons reattach the arteries to the arch.
- Ascending Aorta Repair: In cases where the tear is located in the ascending aorta (the portion of the aorta that is closest to the heart), an open surgical procedure is performed. The procedure involves replacing the damaged section of the aorta with a synthetic graft or tube.
- Descending Aorta Repair: For dissections that occur in the descending aorta (the portion of the aorta that runs through the chest and abdomen), the damaged segment can be replaced or repaired using open surgery techniques.
- Frozen Elephant Trunk Procedure: This procedure is used for complex aortic pathologies that involve both the ascending (near the heart), arch, and descending (farther down the chest and into the abdomen) segments of the aorta. The surgeon will repair or replace the damaged portion of the aorta. The "elephant trunk" component of the procedure involves a stent to cover the portion of the aneurysm that extends into the descending aorta. The stent graft helps to divert blood away from the dissected portion of the aorta. The term "frozen" in "frozen elephant trunk" refers to the fact that the distal end of the stent graft (the part that extends into the descending aorta) is positioned and secured within the aorta, effectively "freezing" it in place.
Thoracic Endovascular Repair of Aorta (TEVAR)
Thoracic endovascular aortic repair (TEVAR) is a minimally invasive procedure used to repair a thoracic aortic aneurysm or dissection. TEVAR is an alternative to open surgery and can mean a shorter hospital stay and quicker recovery time. Since its approval by the Food and Drug Administration (FDA) in 2005, researchers have also documented better patient outcomes with TEVAR compared with open surgical repair.
Malperfusion Management
Malperfusion syndrome, or lack of blood supply to vital organs, is the second most common lethal complication of acute aortic dissection following rupture. It occurs in 10% to 33% of all cases of both acute type A and type B dissection. Early diagnosis is essential. Patients who are at the highest risk of fatality from malperfusion are those with delayed diagnosis of dissection or delayed presentation to a medical center equipped to handle acute aortic dissection.
Malperfusion syndrome occurs when an aortic dissection blocks an artery that carries blood to a vital organ. Twenty years ago, Frankel Cardiovascular Center surgeons developed a world-renowned procedure using a laser inserted through a catheter to make holes in the blockages. This standard of care procedure restores blood flow, enabling surgical repair of the dissection and greatly improves survival.
Medical Management
Medical management of chronic aortic dissections is focused on long-term care and aims to prevent complications, reduce symptoms, and maintain overall cardiovascular health. Chronic aortic dissections are those that have persisted for several weeks or months and are no longer in the acute phase. The management plan may include the following components:
- Blood Pressure Control: Maintaining stable blood pressure is essential to prevent the progression of the dissection and the risk of complications. Patients are typically prescribed blood pressure medications, such as beta-blockers and/or ACE inhibitors, to control hypertension. Blood pressure goals are individualized and may vary based on the extent of the dissection and the patient's overall health.
- Regular Follow-Up: Patients with chronic aortic dissections require regular follow-up appointments with a cardiovascular specialist. These visits are crucial for monitoring the progression of the dissection, assessing the stability of the aortic wall, and adjusting medication as needed.
- Imaging Studies: Periodic imaging studies, such as computed tomography angiography (CTA), magnetic resonance imaging (MRI), or transthoracic echocardiography (TTE), are performed to evaluate the status of the aortic dissection. These tests help determine whether the dissection has expanded or if there are any new developments.
- Pain Management: Chronic aortic dissections can cause persistent or recurrent chest or back pain. Pain management may involve the use of medications, physical therapy, or other pain relief techniques to improve the patient's quality of life.
- Cholesterol Management: Managing cholesterol levels is essential for overall cardiovascular health. Statin medications may be prescribed to lower cholesterol levels and reduce the risk of atherosclerosis, which can contribute to further complications.
- Smoking Cessation: Smoking is a significant risk factor for cardiovascular disease, and patients are encouraged to quit smoking to reduce their risk of complications and improve their overall health.
- Lifestyle Modifications: Patients are advised to make healthy lifestyle changes, including a heart-healthy diet, regular exercise, and weight management. These measures help maintain cardiovascular health and reduce the risk of complications.
- Management of Associated Conditions: Patients with chronic aortic dissections often have comorbid conditions, such as high blood pressure, diabetes, or coronary artery disease. These conditions require appropriate management and control.
- Psychological Support: Living with a chronic condition like aortic dissection can be emotionally challenging. Patients may benefit from psychological support, counseling, or support groups to help them cope with stress and anxiety.
- Regular Aortic Imaging: Depending on the patient's condition, regular imaging of the aorta may be recommended to monitor any changes and assess the need for further intervention.
It's important to note that the management of chronic aortic dissections is highly individualized, and treatment plans may vary from patient to patient.
Make an Appointment
To schedule an evaluation with a Frankel Cardiovascular Center physician, call 888-287-1082. Or visit the Make a Cardiovascular Appointment page to learn what to expect when you call us.
Physicians: To refer a patient, call M-Line at 800-962-3555.

