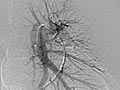
Angiogram of the Lung
Test Overview
An angiogram of the lung is an X-ray, Opens dialog test that uses a special dye and camera (fluoroscopy, Opens dialog) to take pictures of the blood flow in the blood vessels of the lung, Opens dialog.
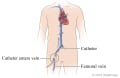
During an angiogram, a thin tube called a catheter is placed into a femoral blood vessel, Opens dialog in the groin (femoral vein) or just above the elbow (brachial vein). The catheter is guided to the area to be studied. Then an iodine dye (contrast material, Opens dialog) is injected into the vessel to make the area show clearly on the X-ray pictures. The angiogram pictures can be made into regular X-ray films or stored as digital pictures in a computer.
A lung (pulmonary) angiogram is used to check the arteries that lead to the lungs (pulmonary arteries) and the blood vessels in the lungs. It can also find narrowing or a blockage in a blood vessel that slows or stops blood flow.
A lung angiogram may be done to measure the pressure in the blood vessels carrying blood to the lungs, to look for lung problems, or to find other causes of blockage or narrowing of the vessels.
Do not eat or drink for 4 to 8 hours before the angiogram. You may be asked to not take aspirin, aspirin products, or blood thinners for several days before the test and for 1 day after the test. If you take these medicines, talk with your doctor.
This test can be done as an inpatient or outpatient. If you are an outpatient, you will stay in a recovery room for several hours before you go home. You may want to bring something to do or read to pass the time. Arrange to have someone take you home because you may get a sedative, Opens dialog before the test. If you stay overnight in the hospital, you will probably go home the next day.
The test may take several hours, so you will empty your bladder just before it starts.
Before the angiogram you may have other blood tests. These include blood clotting (coagulation) studies, blood urea nitrogen (BUN), and creatinine.
If you are breast feeding, use formula (throw out your breast milk) for 1 to 2 days after the angiogram until the dye has passed from your body. This generally takes 24 hours.
An angiogram, Opens dialog can be done by different types of doctors, including a radiologist, Opens dialog, cardiologist, Opens dialog, or surgeon. Your doctor may be helped by a radiology technologist or a nurse.
You will need to take off any jewelry. You may need to take off all or most of your clothes. You will be given a gown to wear during the test.
During the test
You will likely have an intravenous (I.V.), Opens dialog line in a vein in your arm so your doctor can give you medicine or fluids if needed. A device called a pulse oximeter, which measures oxygen levels in your blood, may be clipped to your finger or ear. Small pads or patches (electrodes) are placed on your arms, chest, or legs to record your heart rate and rhythm.
You will lie on your back on an X-ray table. Ask for a pad or blanket to make yourself comfortable. A strap, tape, or sandbags may be used to hold your body still. A lead apron may be placed under your genital and pelvic areas to protect them from X-ray exposure.
A round cylinder or rectangular box that takes the pictures during fluoroscopy will be moved above you. The fluoroscope will move under you during the test.
The place where the catheter will be inserted (in the groin or above the elbow) will be shaved and cleaned. Your doctor will numb the area with a local anesthetic, Opens dialog. Then he or she will put a needle into the blood vessel. A guide wire will be put through the needle into the blood vessel and the needle will be removed. The catheter will be placed over the guide wire and moved into the blood vessel. The catheter will be guided through the blood vessels until the tip is in the area to be studied. Your doctor will use the fluoroscope to watch the movement of the catheter in the blood vessels.
When the catheter is in place, the dye is injected through it. You may be asked to take a breath and hold it for several seconds. Several X-ray pictures will be taken one after another. These will be available right away for your doctor to look at. You need to lie very still so the pictures are clear. Sometimes only one lung is studied, or the process may be repeated more than once for each lung.
An angiogram takes 1 to 2 hours.
After the test
The catheter is taken out after the angiogram, and pressure is put on the needle site for 10 to 15 minutes to stop any bleeding. Then the area may be covered with a bandage or compression device. This will prevent bleeding. You will be given pain medicine if you need it.
If the catheter was put in your groin, you will need to lie still and keep your leg straight for several hours. The nurse may put a weighted bag on your leg to keep it still. If the catheter was put in your arm, you may be able to sit up and get out of bed right away. But you will need to keep your arm still for at least 1 hour.
The place in your hands and feet where your heartbeat (peripheral pulse) can be felt may be marked with a pen. Your pulse may be checked before and after the angiogram.
You may feel a brief sting or pinch from the numbing medicine. Most people do not have pain when the catheter is in the blood vessel.
You may feel pressure in the blood vessel as the catheter is moved. Let your doctor know if you are having pain.
You will probably feel some warmth when the dye is put in. This feeling lasts only a few seconds. For some people, the feeling of heat is strong and for others it is very mild.
You may feel a need to cough but try to keep holding your breath until you are told to breathe.
You may have a headache, flushing of the face, or a salty or metallic taste in your mouth after the dye is used. These feelings do not last long. Some people may feel sick to their stomach or may vomit, but this is not common.
After the test, you may have some tenderness and bruising at the site where the catheter was inserted.
You can drink extra fluids to pass the dye from your body unless your doctor has told you not to.
The chance of any major problem from an angiogram is very small, but some problems can occur. In most cases the problems occur within 2 hours after the test when you are in the recovery room. If the problem occurs during the angiogram, the test may not be completed. You may need urgent treatment that could include surgery.
- There is a chance of an allergic reaction, Opens dialog to the iodine dye. The reaction can be mild (itching, rash) or severe (trouble breathing or sudden shock). Most reactions can be treated with medicines. Be sure to tell your doctor if you have hay fever, asthma, or iodine allergy or food allergies.
- Bleeding from the needle site may occur. Also, a blood clot can form where the catheter was inserted. This may cause some blockage of the blood flow from the arm or leg.
- The iodine dye used for the test can cause water loss or direct damage to the kidneys. This is a special concern for people who have kidney problems, diabetes, or who are dehydrated, Opens dialog. Special measures are used during the test to prevent problems for people who need an angiogram and have these conditions.
- There is always a small chance of damage to cells or tissue from being exposed to any radiation, even the low level used for this test.
Your doctor may tell you some results right after the test. Full results are usually ready the same day.
Normal: | The dye flows evenly through the blood vessels. |
|---|---|
No narrowing, blockage, bulging, or other problem of the blood vessels is seen. The pulmonary artery pressures are normal. | |
Abnormal: | Blood vessels that are not in their normal position may mean that a tumor or other growth is pushing against them. |
A bulge in a blood vessel may mean a weakness in the blood vessel wall (aneurysm, Opens dialog). | |
Dye, Opens dialog that leaks out of a blood vessel may mean there is a hole in the blood vessel. | |
There is an abnormal vessel or blockage between vessels in the lung. | |
There is abnormal branching of blood vessels present since birth (congenital). |
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.